The Prior Authorization (PA) process has long stood as a frustrating barrier in U.S. healthcare, notorious for delaying patient care, exhausting provider resources, and imposing massive administrative costs on payers. This systemic inefficiency stems from reliance on fragmented, analog, and unstructured data exchanges. In response, the CMS Interoperability and Prior Authorization Final Rule now mandates accelerated decision-making—72 hours for expedited requests and seven calendar days for standard requests—and requires specific, auditable denial rationales. To meet these strict new requirements and achieve meaningful automation, healthcare payers and utilization management (UM) vendors are adopting a sophisticated, integrated solution: Agentic AI powered by the HL7 FHIR Da Vinci Burden Reduction APIs.
This integration is not simply an upgrade; it’s a fundamental restructuring that creates an automated, end-to-end workflow, turning a cumbersome administrative process into a seamless digital transaction.
The Significance of FHIR: The Language of Automation
To understand the power of agentic AI, one must first grasp the critical significance of the HL7 Fast Healthcare Interoperability Resources (FHIR®) standard. In the era preceding FHIR, clinical documentation was a chaotic mix of vendor-specific proprietary data models, scanned faxes, and free-text notes. When an AI attempted to consume this data using only Natural Language Processing (NLP), it faced an “inconsistent data translation” crisis.
Without FHIR, AI struggles with what can be termed the “unstructured data crisis,” which creates severe administrative failures:
- Semantic Ambiguity: Clinical documents use varied free text and abbreviations. The lab value of “7.5” is meaningless without units or context, leading to high error rates and incorrect medical necessity assessments.
- Syntactic Variability: Every EHR vendor structures its data differently, meaning the AI would have to be re-trained for every single provider system, rendering national automation unscalable.
- Lack of Context/Metadata: Unstructured notes lack required metadata like the specific ICD-10/SNOMED code or the date of observation. This prevents the AI from confirming time-sensitive criteria, resulting in policy incompliance.
FHIR solves this by providing universal, standardized blueprints for health data. It defines clear data containers called Resources (Patient, Condition, Observation, Claim, etc.) and requires the use of standardized code systems (like SNOMED CT and LOINC). This structure is foundational:
- Standardized Resources provide consistency, ensuring the AI knows that Prior Authorization Submission data will always be a FHIR Claim resource regardless of the source.
- Terminology Binding provides semantic clarity, ensuring that when the AI extracts “Diabetes,” it is bound to a specific ICD-10 code, allowing clinical criteria checks with zero ambiguity.
The Engine: Agentic AI and the Da Vinci Workflow
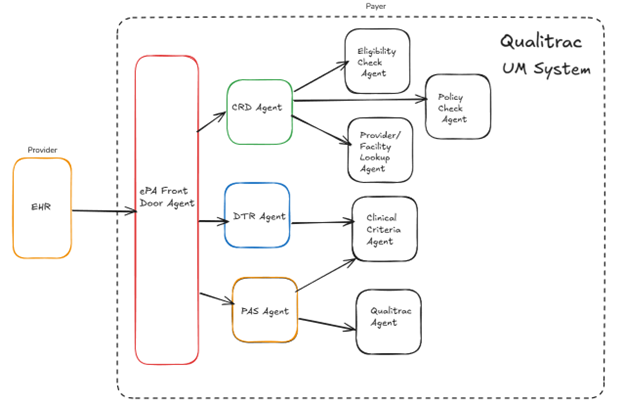
Agentic AI goes beyond simple automation; it involves autonomous, goal-driven systems designed to perceive the digital environment, reason against complex policies, and execute actions. The agentic AI system acts as the intelligent engine that drives the entire electronic prior authorization (e-PA) lifecycle across the three mandated FHIR APIs: Coverage Requirements Discovery (CRD), Documentation Templates and Rules (DTR), and Prior Authorization Support (PAS).
The use of AI agents is vastly more efficient than relying solely on plain API calls, which are limited to syntax only and fixed, reactive rules. The AI agent provides adaptive reasoning and autonomy:
- Agentic AI is autonomous and proactive: It orchestrates the entire workflow without requiring a human to initiate each step, and it can handle missing data or exceptions by autonomously retrieving more information.
- It interprets context and semantics: It uses LLMs to consume clinical data, moving beyond fixed rules to understand nuanced clinical guidelines.
- It makes data mapping between the FHIR standard and Payer/UM system seamless.
e-PA Step 1: Coverage Requirements Discovery
The process begins proactively at the provider’s point of care, eliminating unnecessary submissions. When a provider orders a service within their Electronic Health Record (EHR), the system automatically triggers a request using the Coverage Requirements Discovery (CRD) protocol. An agentic AI in the payer/Utilization Management (UM) system instantly ingests the incoming FHIR message, performs an eligibility check, conducts provider/facility lookup, and determines whether authorization is required against the payer’s fee schedule. The agent immediately sends a Clinical Decision Support (CDS) Hook response back to the EHR, informing the provider of the requirements, thus reducing administrative waste.
e-PA Step 2: Documentation Templates and Rules
If authorization is required, the AI agent shifts to directed data collection using the Documentation Templates and Rules (DTR) API. The payer agent sends the provider a specialized FHIR Questionnaire resource that is a dynamic, logic-based form tailored to the specific service and the individual patient. This is the crucial point where agentic AI excels:
- DTR uses Clinical Quality Language (CQL) to define what data is needed (the simple FHIR query) and automatically pre-populate the required structured evidence into the Questionnaire.
- This ability ensures the submission is complete and accurate the first time.
e-PA Step 3: Prior Authorization Support
The final step is the electronic submission and automated decision-making facilitated by the Prior Authorization Support (PAS) API, which is directly responsible for meeting the CMS time mandates. The provider submits the complete request as a structured FHIR Claim Bundle. The back-end agentic AI system then performs the core adjudication. It compares the structured patient evidence against the clinical guidelines. For a significant volume of submissions, the system achieves touchless adjudication—approving the request instantly.
The agent generates the final decision as a FHIR ClaimResponse Bundle. This response is critical for CMS compliance: the automated nature ensures the 72-hour and seven-day deadlines are consistently met.
Conclusion: The Future of Utilization Management
The combination of agentic AI and the FHIR Da Vinci APIs is redefining utilization management. It moves the payer-provider relationship out of the fax era and into a world of instantaneous, intelligent, and transparent digital exchange. While the FHIR APIs provide the essential plumbing and standard data format, the agentic AI provides the brain and the autonomy needed to execute complex policy reasoning. By leveraging FHIR’s consistency to feed high-quality data into an agentic AI engine that drives the logic of the three APIs, payers can not only comply with the CMS Final Rule but also unlock massive operational benefits. This system reduces administrative costs, drastically cuts denial rates due to incomplete documentation, and, most importantly, accelerates the delivery of necessary care to the patient. This digital transformation marks a critical step toward a more efficient, interoperable, and patient-centered healthcare ecosystem.

