The Gravity Project, an HL7 FHIR Accelerator and multistakeholder collaborative creating consensus-based SDOH data standards, has become the reference standard for social determinants of health (SDOH) interoperability across the country. Its work is now reflected in federal guidance and national quality frameworks, including CMS Medicaid policy encouraging states to align with Gravity standards, ONC’s HTI-1 Final Rule, and the United States Core Data for Interoperability (USCDI). National accreditation and measurement bodies such as NCQA also reference Gravity value sets for emerging health equity, social needs screening and intervention measures. As health systems, payers and public agencies increasingly recognize the importance of addressing SDOH, states are taking significant steps to standardize how data to address the social determinants of health are collected and exchanged.
Gravity in State Guidance and Regulation
Several states have already formally embedded Gravity standards into their policy and planning frameworks. While many others are leveraging Gravity-aligned terminology through pilots and data exchange efforts, the following states have taken the lead in codifying Gravity into official policy or strategy documents:
- New York: Gravity terminology and the SDOH Clinical Care FHIR Implementation Guide underpin New York’s 1115 Medicaid waiver and Social Care Network design.
- Nebraska: The Nebraska Health Information Technology Board’s Social Care Data Standards Specification and its SDOH Playbook align with Gravity Project value sets and referral management standards.
- Michigan: The MI Department of Health and Human Services Office of Policy & Planning explicitly references the Gravity Project as the national standard for social needs screening and documentation in their statewide SDOH Strategy, Michigan’s Roadmap to Healthy Communities, emphasizing its role in promoting consistent data collection and health equity insight.
- Colorado: The Colorado Office of eHealth Innovation (OEHI) has incorporated Gravity Project standards into its statewide Social Health Information Exchange (CoSHIE) initiative. According to program leadership at the September meeting of the Health IT Data Governance Work Group of the eHealth commission, the state’s vendor contract for the CoSHIE platform includes explicit requirements to implement Gravity-aligned SDOH terminology and FHIR-based exchange standards. While formal documentation has not yet been published, CoSHIE’s implementation reflects Colorado’s commitment to grounding SDOH interoperability in nationally recognized Gravity standards.
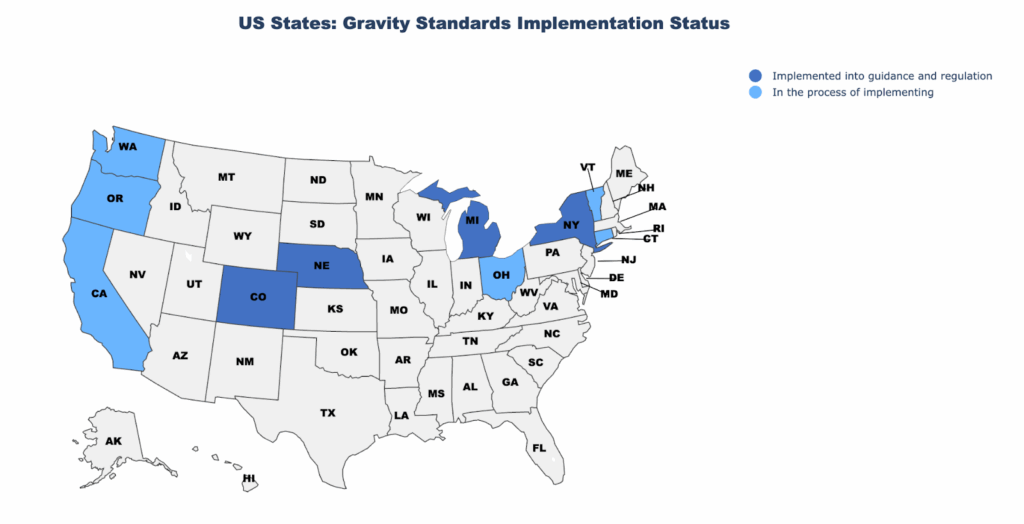
Figure 1: Implementation Status of Gravity SDOH Standards by US State
States to Watch
Several additional states are actively exploring or preparing to implement Gravity standards, signaling broader nationwide alignment:
- California: The California Data Exchange Framework (DxF) calls for 2025 adoption of minimum data elements and technical specifications for social services data exchange “in accordance with emerging standards from Gravity/FHIR.”
- Washington: The Department of Health’s 2025 FHIR Infrastructure Roadmap names the Gravity SDOH Clinical Care IG as a core interoperability standard for community and clinical data exchange.
- Oregon: Oregon’s HIE Workgroup in its paper “Demonstrating Value with Social Determinants of Health Use Cases of HIE” refers to the HL7 Gravity Project as part of how SDOH data is beginning to be included in federal standards. While this is more of a concept/strategy document than a binding law, it shows that the state is considering Gravity Project standards in its planning for HIE / interoperability architecture.
- Connecticut: The 2022–2026 Statewide Health IT Plan highlights the Gravity Project as the industry best practice for standardizing social needs assessments and interoperability frameworks.
- Ohio: In Ohio, the effort to align with the Gravity Project standards around health‑related social needs (HRSN) is clearly embedded in the state’s policy roadmap. The Health Policy Institute of Ohio (HPIO) report emphasizes the need for a statewide data infrastructure that includes data standards for housing, nutrition, care coordination and other HRSN services, noting explicitly that Ohio is “considering the Gravity Project as a national resource in data standards.”
- Vermont: The Vermont Social Determinants of Health (SDOH) Roadmap explicitly references the Gravity Project as the leading national framework for SDOH terminology and data exchange. The report recommends that Vermont’s Unified Health Data Space (UHDS) and Health Information Exchange (VHIE) governance bodies align data and technical standards with Gravity’s terminology value sets and FHIR SDOH-CC Implementation Guide as a key milestone.
Why It Matters
By integrating Gravity standards into guidance and regulation, states are not only improving interoperability but also aligning with broader national drivers such as USCDI, federal screening requirements, and NCQA quality measures. This alignment ensures that social needs data are actionable, comparable, and applicable across sectors, helping states advance multiple priorities at once: targeting interventions, measuring outcomes, and connecting communities with essential services.
“Due to the scale and speed of the 1115 Waiver implementation in NY, it was critical to be able to integrate screenings coming from a wide variety of healthcare partners. To ensure interoperability, NY sought to leverage Gravity standards in the exchange of these screenings to ensure IT Platforms (i.e., UniteUs, FindHelp and Channels360) were able to ingest those FHIR compliant screenings in real-time for a navigator to complete referrals. The Gravity Project supported the implementation of existing standards in NY, as well as the development of new terminology for specific services and workflows that would be valuable to other Gravity partners.”
- New York eHealth Collaborative on their implementation of Gravity’s SDOH Clinical Care Implementation Guide
Looking Ahead
As states continue to modernize their data infrastructure, more will likely follow the lead of early adopters, embedding Gravity terminology and FHIR-based exchange frameworks into regulations, Medicaid programs and HIE/CIE initiatives. The growing state momentum underscores Gravity’s role as the national reference point for interoperability of data to address the social determinants of health. The Gravity Project SDOH Clinical Care Implementation Guide STU 2.3 is now available, with STU 3.0 planned for ballot in January 2026.
